Do not take MAVENCLAD if you:
- have cancer (malignancy).
- are pregnant, plan to become pregnant, or are a woman of childbearing age or a man able to father a child and you are not using birth control.
- are breastfeeding.
- are human immunodeficiency virus (HIV) positive.
- have active infections, including tuberculosis (TB), hepatitis B or C.
- are allergic to cladribine.
Before you take MAVENCLAD, tell your healthcare provider about all of your medical conditions, including if you:
- think you have an infection.
- have taken, take, or plan to take medicines that affect your immune system or blood cells, or other treatments for MS. Certain medicines can increase your risk of getting an infection.
- have had a recent vaccination or are scheduled to receive any vaccinations. You should not receive live or live-attenuated vaccines within the 4 to 6 weeks preceding treatment with MAVENCLAD or receive these types of vaccines during your treatment with MAVENCLAD and unless directed by your healthcare provider.
- have heart failure.
- have or have had cancer.
- have liver or kidney problems.
- are breastfeeding or plan to breastfeed. It is not known if MAVENCLAD passes into your breast milk. Do not breastfeed on the days on which you take MAVENCLAD, and for 10 days after the last dose.
How should I take MAVENCLAD?
- MAVENCLAD is given as two yearly treatment courses, consisting of 2 treatment weeks (cycles) about a month apart.
- Handle MAVENCLAD with dry hands and take immediately after opening the blister pack. Take with water and do not chew the tablet. MAVENCLAD can be taken with or without food and should be taken at least 3 hours apart from other medicines.
- Wash your hands after handling MAVENCLAD. Limit contact with your skin (especially on your face). Wash skin and surfaces with water if contact occurs.
- If you miss a dose, take it as soon as you remember on the same day. If the whole day passes before you remember, take your missed dose the next day. Do not take 2 doses at the same time. Instead, you will extend the number of days in that treatment week.
Your healthcare provider will continue to monitor your health during the 2 yearly treatment courses, and for at least another 2 years during which you do not need to take MAVENCLAD. It is not known if MAVENCLAD is safe and effective in people who restart MAVENCLAD treatment more than 2 years after completing 2 yearly treatment courses.
MAVENCLAD can cause serious side effects. If you have any of these symptoms listed below, call your healthcare provider right away:
- low blood cell counts have happened and can increase your risk of infections during treatment with MAVENCLAD. Blood tests are needed before you start treatment with MAVENCLAD, during your treatment with MAVENCLAD, and afterward, as needed.
- serious infections such as:
- life-threatening or fatal infections caused by bacteria, viruses, parasites or fungi.
- TB, hepatitis B or C, and shingles (herpes zoster). Fatal cases of TB and hepatitis have happened with cladribine during clinical studies. Tell your healthcare provider right away if you get any symptoms of the following infection related problems or if any of the symptoms get worse, including fever, aching painful muscles, headache, feeling of being generally unwell, loss of appetite, burning, tingling, numbness or itchiness of the skin in the affected area, skin blotches, blistered rash, or severe pain.
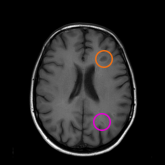
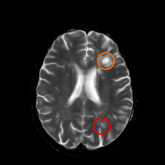
- progressive multifocal leukoencephalopathy (PML). PML is a rare brain infection that usually leads to death or severe disability. Although PML has not been seen in MS patients taking MAVENCLAD, it may happen in people with weakened immune systems. Tell your healthcare provider right away if you have any new or worsening neurologic signs or symptoms. These may include: weakness on 1 side of your body, loss of coordination in your arms and legs, decreased strength, problems with balance, changes in your vision, changes in your thinking or memory, confusion, or changes in your personality.
- liver problems. Symptoms of liver problems may include: nausea, vomiting, stomach pain, tiredness, loss of appetite, dark urine, or your skin or the whites of your eyes turn yellow. Your doctor will perform blood tests to check your liver during treatment.
- allergic reactions (hypersensitivities). You should stop treatment and seek immediate medical attention if any signs or symptoms of allergic reactions occur. Symptoms of an allergic reaction may include skin rash, swelling or itching of the face, lips, tongue or throat, or trouble breathing.
- heart failure. MAVENCLAD may cause heart failure, which means your heart may not pump as well as it should. Call your healthcare provider or go to the closest emergency room for medical help right away if you have any signs or symptoms such as shortness of breath, a fast or irregular heartbeat, or unusual swelling in your body.
The most common side effects of MAVENCLAD include: upper respiratory infection, headache, and low white blood cell counts.
These are not all the possible side effects of MAVENCLAD. Call your doctor for medical advice about side effects. To report SUSPECTED ADVERSE REACTIONS, contact EMD Serono at: 1-800-283-8088 ext. 5563 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Please see full Prescribing Information and Medication Guide, including serious side effects.